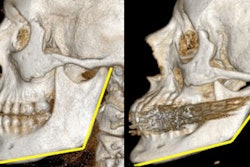
New research by University of Cincinnati oral and maxillofacial surgeons suggests that treating isolated lower mandibular fractures on an outpatient basis has the same outcome and significantly lowers healthcare costs.
Michael Grau, D.M.D., will present findings from his study, "Safety and cost-efficiency in treating mandibular fractures nonemergently," this week at the 2010 meeting of the American Association of Oral and Maxillofacial Surgeons (AAOMS) in Chicago.
To conduct this research, Dr. Grau examined 440 cases of lower jaw fractures, all treated by the University of Cincinnati division of oral and maxillofacial surgery between July 2004 and June 2009.
He divided patients into groups based on how soon they received care after their injury (zero to 72 hours, three to seven days, and more than seven days) and then evaluated the cases for the presence of complications requiring a return trip to the operating room.
"A complication could be anything from an infection that requires surgical draining to a removal of infected hardware or a fracture that didn't heal properly," Dr. Grau said in a news release. Anything that could be treated with a minor outpatient visit to the doctor was not counted as a complication.
"The main thing we were looking at was the complication rate in relation to how quickly they were treated after their initial injury, looking for any differences between patients treated immediately and those treated days after," he said.
What they found was little to no difference in complication rate among groups -- meaning that jaw fracture patients can be treated on a nonemergency or outpatient basis without increasing the risk of further complications.
Cost reductions
Admitting patients into the hospital immediately after injury does not always guarantee faster treatment, noted Deepak Krishnan, D.D.S., assistant professor of surgery and residency program director at the university.
"Depending on the time of their injury and admittance, sometimes patients can wait several hours, sometimes days to get into surgery," he said. "That causes a great deal of stress for the patient. You can't eat or drink anything before surgery -- and often the surgery will be delayed if surgeons are called to more urgent cases."
Sending the patients home with adequate pain coverage and antibiotics allows them to avoid the stress of a hospital stay and return to receive scheduled treatment at a location convenient to them. It also reduces costs for healthcare providers.
"There's no nursing cost for an overnight hospital stay, there's no cost for treatment of hospital stay-associated complications. ... The cost was dramatically improved with no difference in outcome," Dr. Krishnan said.
In addition, the cases studied were at the university's Health University Hospital, a level I trauma center, he noted. "So we are seeing the worst of the worst cases, the ones that could potentially have all of the possible complications," he said. "We've shown in five years of experience that outpatient care is a very acceptable way of treating them, without any adverse effects on the outcomes."
Oral and maxillofacial surgery researchers from the University of Cincinnati will present three other abstracts at the AAOMS conference, including work on trends in antibiotic usage about facial trauma providers, cleft lip/palate surgery, and treatment of cysts in the orofacial region.
Copyright © 2010 DrBicuspid.com