
Microchips that mimic parts of the human body may sound futuristic, but these devices -- called organs-on-chips -- are already being used to study human biology. Made from plastic, with grooves that are lined with cells and channels that transport air and fluids, these chips can simulate aspects of organ structure and function.
Chips have been designed to mimic many different parts of the body, including beating heart tissue, air-filtering lung cells, and electrically active brain cells. The technology could help accelerate drug discovery, enable personalized medicine, and even reduce the need for animal experiments.
Researchers on projects supported by the U.S. National Institute of Dental and Craniofacial Research (NIDCR) are taking advantage of the technology, putting parts of our mouths on chips to find better ways to treat oral diseases. From tooth-on-a-chip studies at Oregon Health & Science University (OHSU) to a salivary gland chip development at the University of Rochester and more, scientists are testing dental materials, repurposing drugs for salivary gland dysfunction, and peering into the inner workings of the oral cavity.
In the early stages of human disease research, scientists carry out studies in animals or cells that are cultured in a petri dish. However, findings from animals don't always translate to humans, and cells may behave differently in a two-dimensional dish than they would in the human body. Organs-on-chips, also known as tissue chips, occupy a unique niche between living systems and cultured cells, creating an environment for tissues to grow three dimensionally and display more lifelike responses.
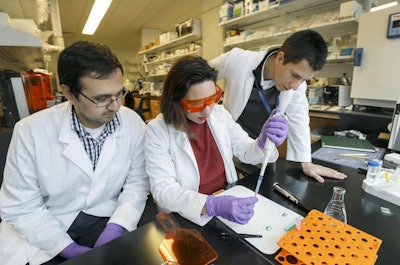 Luiz Bertassoni (far right) and his team developed a miniature tooth system to closely observe the interactions among dental materials, the microbiome, and tooth tissue. Image courtesy of Oregon Health & Science University.
Luiz Bertassoni (far right) and his team developed a miniature tooth system to closely observe the interactions among dental materials, the microbiome, and tooth tissue. Image courtesy of Oregon Health & Science University."In a way, we are putting a window on the tissue, and we can watch how it responds," says OHSU's Dr. Luiz Bertassoni, PhD. A couple years ago, Bertassoni's team designed their first tooth-on-a-chip to understand how microbes and biomaterials such as dental fillings interact with teeth.
The group's stamp-sized chip consists of a thin slice of a human molar sandwiched between two chambers. One chamber, representing the interior of the tooth, contains dental pulp, which is made up of cells that keep the tooth vital; the other chamber mimics the outside of the tooth, where it comes into contact with oral bacteria and dental materials.
While scientists had extensively studied dental materials in animals and cell culture, they hadn't fully understood how the cells inside a real human tooth react. Using their newly developed tooth-on-a-chip, Bertassoni's team set out to fill that gap in a 2020 study published in Lab on a Chip. On the surface of the molar slice, the team applied an acid, primer, and adhesive -- materials used for standard tooth restorations, such as fixing dental caries and chipped teeth.
Using a microscope to peer through the chip's transparent rubber casing, the researchers watched as the pulp responded in real time to the materials applied to the tooth slice. As soon as 24 hours after the application, the scientists observed changes in the pulp cells' shape and structure. Importantly, the team found evidence of potential harm, as the restoration materials were able to reach, damage, and even kill pulp cells by permeating through tiny tube-like structures in the tooth slice.
"Some of these treatments are done millions of times in a single day across the globe, and I didn't expect the effect on the cells would be so noticeable," says Bertassoni.
In a study published the following year in the Journal of Dental Research, his team found that applying different restorative materials with biologically active properties promoted pulp cell growth and quelled tooth decay-causing bacteria on the tooth chip. The studies demonstrated how the system could aid study of the tooth interface and generate insights into how dental materials affect tooth genetics, health, and survival.
Bertassoni envisions that the chip could help lead to the development of less-damaging dental materials and open doors to personalized dentistry, where clinicians could design a chip for each patient to tailor individualized treatments.
Danielle Benoit, PhD, of the University of Rochester, and her colleagues, Lisa DeLouise, PhD, and Catherine Ovitt, PhD, are developing salivary gland chips for testing drugs that could protect glands from the side effects of radiation therapy for head and neck cancers.
 Lisa DeLouise (left), Danielle Benoit (right), and Catherine Ovitt (not pictured) developed a tissue chip (above) with bubble-shaped wells that hold tiny salivary glandlike clusters to screen for drugs that protect the salivary glands from radiotherapy for head and neck cancer. Image courtesy of the University of Rochester.
Lisa DeLouise (left), Danielle Benoit (right), and Catherine Ovitt (not pictured) developed a tissue chip (above) with bubble-shaped wells that hold tiny salivary glandlike clusters to screen for drugs that protect the salivary glands from radiotherapy for head and neck cancer. Image courtesy of the University of Rochester."These chips are valuable as a new tool for probing salivary gland function in vitro," says Benoit. Their work is supported by NIDCR as part of the trans-National Institutes of Health (NIH) Tissue Chip for Drug Screening program led by the National Center for Advancing Translational Sciences (NCATS), which aims to develop tissue chips to accelerate the translation of basic discoveries into the clinic.
For head and neck cancer patients, radiation therapy can permanently damage salivary glands, interfering with saliva production and causing chronic dry mouth. Without enough saliva, people may have difficulty eating and speaking, and they are at increased risk for tooth decay and other oral health problems. While clinicians can give a protective drug called amifostine prior to radiotherapy, the side effect -- a dramatic drop in blood pressure -- has steered many patients and clinicians away from its use.
To find better radioprotective drugs, the team at Rochester developed a tissue chip that holds hundreds of tiny, human salivary glandlike cell clusters for rapid drug screening. Each salivary gland cell cluster is suspended in a gellike material and seeded into a fishbowl-shaped microbubble that's smaller than a grain of sand. The unique architecture of the bubbles shapes the clusters to resemble the globelike units that make up real salivary glands. The tiny environment also concentrates vital proteins and other molecules to keep the tissue alive and functioning.
In a 2021 Communications Biology paper, the researchers reported that the salivary gland clusters maintained cell organization, expressed genes, secreted proteins, and responded to fluid-secretion signals much like real salivary glands. They also found that the drug amifostine protected the cell clusters from radiation-induced damage, indicating the potential for salivary gland chips to facilitate large-scale drug studies. Next, the team plans to screen more than 800 compounds approved by the U.S. Food and Drug Administration to find radioprotective drugs that might be repurposed for head and neck cancer patients.
While the OHSU and Rochester teams continue to optimize and validate their chips, other NIDCR-supported studies are developing mouth-related chips as well. Some research groups are crafting chips that mimic oral barrier tissue to understand gum disease, while others are engineering a gum-tissue chip to develop treatments for mouth sores caused by cancer therapy. Another research team is even building a "human"-on-a-chip by integrating tissue from multiple body systems; the project is supported by NIDCR and several other NIH institutes as part of the trans-NIH tissue chip program.
"These chips really have translational potential for discovering something that could impact patient care," says DeLouise. "That motivates me, and that's why I'm excited."
Reprinted from the U.S. National Institutes of Health's National Institute of Dental and Craniofacial Research.



















