Previous studies have found that the use of implants with a rough surface and microthreaded neck may reduce crestal bone loss compared with other implant types, but this positive effect is subject to various factors.
To better determine the effects of this implant design on crestal bone preservation, researchers conducted a systematic review of the published literature on the topic. Dental implants with a microthreaded-neck design are a better choice than other designs, they found.
"The addition of threads or microthreads up to the crestal module of an implant may positively contribute to bone-to-implant contact and to the preservation of marginal bone," wrote lead study author Ahmad Al-Thobity, MDS, and colleagues (Journal of Oral Implantology, April 2017, Vol. 43:2, pp. 157-166).
Dr. Al-Thobity is an assistant professor in the department of substitutive dental sciences at the University of Dammam College of Dentistry in Dammam, Saudi Arabia.
Boning up
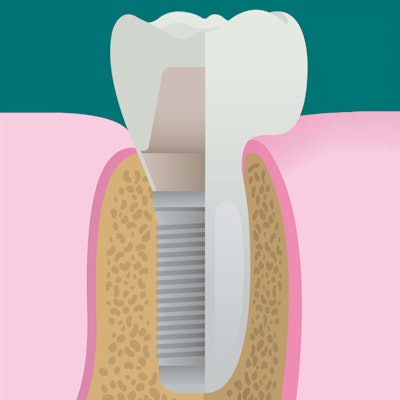
The preservation of bony support around a dental implant is key to long-term clinical success, according to previous research. Several recent studies have found that implants with a rough surface and microthreaded-neck design may improve the preservation and stabilization of crestal bone.
The current generation of implants combine a continuous microrough or nanorough surface extending to the implant neck, which can facilitate osseointegration along the implant's entire length, with microthreads in the cervical region, which can transmit functional loads to the adjacent bony structures and stabilize the region. The researchers of the current study sought to determine if microthreaded-neck implants positively affect crestal bone levels around dental implants based upon published clinical trials.
“The addition of threads or microthreads up to the crestal module of an implant may positively contribute to bone-to-implant contact and to the preservation of marginal bone.”
Many factors can affect the biological behavior of bone and long-term outcomes of these implants, the authors explained. These factors include the following:
- Bone quality and quantity
- Biologic width around the tooth or implant and use of platform switching
- Implant and abutment design at the macro-, micro-, and nanolevel and implant dimensions
- Depth of implant insertion
- Timing of loading and restoration, prosthetic procedures, and frequency of secondary-component replacement
Biologic width refers to the dimensions of periodontal and peri-implant soft-tissue structures, such as the gingival sulcus, junctional epithelium, and supracrestal connective tissues, the authors explained. Platform switching is the concept of using a narrower diameter abutment on a wider diameter implant, which appears to protect the marginal bone and counteract bone resorption tendencies. Conventional positioning, on the other hand, can lead to a microgap between the implant and abutment that is vulnerable to bacterial contamination and can reduce implant stability and cause crestal bone loss.
The researchers searched electronic databases for high-quality, original peer-reviewed clinical studies published from January 1995 and June 2016 that measured crestal bone loss during a reported follow-up period. They required that articles included in their review meet the following criteria:
- Compared microthreaded implants to another implant type
- Used a study design that was a randomized controlled trial, prospective or retrospective cohort study, case control study, cross-sectional study, or another clinical trial design that could answer the main study question
Ultimately, their review included 23 studies, 15 of which were considered by the authors to have a low risk of bias, seven a moderate risk, and one a high risk. The low-risk studies were typically randomized controlled trials, with most other cohort studies considered to have a moderate risk of bias. Of the 23 studies, 15 were prospective and the remainder retrospective. The number of participants in each study ranged from nine to 59.
Crestal bone loss was measured with CT scans in two studies, standardized periapical radiographs in 18 studies, and panoramic radiographs in three studies. The number of microthreaded implants placed in the included studies ranged from 17 to 118. Follow-up was from 12 to 36 months in 18 studies and 40 to 96 months in five studies.
Among the studies, crestal bone loss after loading ranged from 0.05 to 0.9 mm. Measurements varied due to differences in implant systems, loading protocols, types of prostheses, and differences in imaging systems and reference points used, the authors noted.
Eleven studies used Astra Tech implants (Dentsply Implants), which contain pure grade 4 titanium and have a moderately rough surface blasted with titanium dioxide particles and a microthreaded implant collar. The following implants were used in one to three studies: NobelReplace Straight Groovy (Nobel Biocare), Hexplant (Warantec), Implantium (Dentium), MIS (MIS Implants Technologies), Inhex (Mozo-Grau), Osstem (Osstem), and Oneplant (Warantec).
Implants were placed in pristine bone in 18 studies and in fresh sockets in the remainder. Five studies used immediate loading, 17 used conventional loading, and one used both.
Astra Tech implants fabricated and conventionally loaded with fixed partial-denture prostheses produced the smallest crestal bone loss measurements, (0.05 ± 0.11 mm) after follow-up of 12 months. Nonocclusal MIS implants loaded with fixed prostheses after 60 months of follow-up saw the largest measurements at 0.9 ± 0.26 mm. The results of some studies suggest that immediate loading leads to greater crestal bone loss, the authors wrote.
Studies that compared crestal bone loss around microthreaded rough-surface implants and conventional rough-surface implants found greater crestal bone loss with conventional rough-surface implants. Crestal bone loss was also found to be greater in all studies that compared machined-surface with microthreaded rough-surface implants and machined-neck implants compared with microthreaded-neck ones.
A recent study found that implants with a platform-switching design were associated with less crestal bone loss than those with a nonplatform-switching design, the review authors wrote. The results of their systematic review match those of animal studies and finite-element studies, they noted.
Benefits may be minimized
In their review, the authors found a wide variation among the findings and radiographic parameters of the included studies, which could minimize the positive effects of microthreaded-neck implants on crestal bone loss.
Additional randomized controlled trials should be conducted to evaluate crestal bone loss around microthreaded-neck implants in grafted bone, pristine bone, and extraction sockets with various loading protocols and using standardized imaging techniques, they wrote.
"Within the limitation of the present systematic review, the results indicate that thread geometry affects the distribution of stress forces around the implant," the authors concluded. "A decreased thread pitch may positively influence implant stability. Deeper threads seem to have an important effect on stabilization for patients with poorer bone quality."