When it comes to replacing missing teeth, dental implants improve quality of life, but fixed partial dentures may prove more cost-effective over time. These findings come from a new study evaluating the cost-effectiveness of different treatments to replace missing lower molars.
Researchers from Japan studied the long-term costs and quality of life for patients who received implants, fixed partial dentures, and removable partial dentures. They published their findings in BMC Oral Health (August 20, 2018).
"To date, there has been little economic assessment research using the measurement of oral quality of life, which is widely used worldwide in relation to the effect," wrote the authors, led by Arai Korenori from the department of oral implantology at Osaka Dental University. "This study thus aims to undertake a cost-effectiveness analysis of the prosthetic treatment for the intermediate loss of a single molar."
Comparing cost and quality of life
Health technology assessments are the systematic evaluation of medical technologies from economic, social, ethical, and organizational perspectives. The goal of these assessments is to provide a scientific base of knowledge upon which policymakers can make medical care policies designed to achieve the best value for care.
However, while the assessments are fairly prominent in medicine, there is a lack of these analyses investigating dental technology. Therefore, the researchers decided to conduct their own health technology assessment to study the cost-effectiveness and quality of life effect of technologies used to treat the loss of a single molar.
They based their cost research on the modern-day health insurance landscape in Japan. Currently, the Japanese universal health insurance system covers dentures that are made of metals, such as gold, silver, and palladium. However, dental implants and dentures using other materials, such as porcelain or ceramic, are not covered by insurance and must be paid for out of pocket.
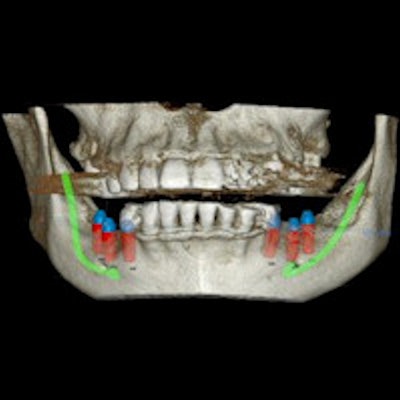
The researchers were curious whether it was more cost-effective for patients to use an insurance-funded fixed partial denture or to pay out of pocket for a privately funded denture or implant. To find out, they asked 560 patients who had lost a molar in their lower jaw to complete an oral health quality of life survey. The patients received an implant, fixed dental prosthetic (FDP), removable dental prosthetic (RDP), or no treatment at the Osaka Dental University Department of Oral Implantology.
Oral health quality of life (QOL) was determined by converting a general oral health assessment index score to a numerical value between 0 and 1, with 0 as the least satisfied and 1 as the most satisfied. The average QOL value for the Japanese population ages 50 to 59, the median range among survey participants, is 0.84 using the researcher's scale.
| Quality of life scores for various treatments | |
| Treatment | Score |
| Successful implant | 0.88 |
| National average | 0.84 |
| Successful FDP | 0.83 |
| Failed implant to FDP | 0.71 |
| RDP | 0.71 |
| Failed FDP to RDP | 0.68 |
Patients who received successful implants reported the highest oral health quality of life, followed by the Japanese national average and those who received successful fixed partial dentures. Patients with failed implants, failed fixed partial dentures, and removable partial dentures reported a lower oral health quality of life.
"Comparing with this result, the results of the current study can be considered the same as implants and FDP that perform well over time," the authors wrote. "That is, lost implants and removed FDP do not function as well as national norms."
After cost analysis, insurance-funded dental prosthetics provided great cost-effectiveness for patients who were less willing to pay out of pocket. Implants also were considered to be cost-effective, but they cost 1,850 euros ($2,150) more than fixed partial dentures funded by insurance.
"In this study, starting with an implant for the prosthetic treatment of a single missing tooth in the molar region of the lower jaw had a higher QOL condition than either [insurance-paid or privately funded fixed dental prosthetics]," the authors wrote. "However, [insurance-funded prosthetics] had the lowest cost among the three groups when estimated for 30 years."
More data needed
The study had a number of shortcomings, including that it relied on three previous studies to determine what treatment followed failed implants and fixed dental prosthetics. Furthermore, it only accounted for quality of life after one treatment failure, and the researchers could not assess the condition of patients' other teeth or gums.
In addition, the authors were concerned that dental institutions in Japan are not collecting enough data to robustly study the cost-effectiveness of implants. They hope that this changes in the future.
"In terms of the advancement of clinical research, construction of a database that permits identification and access to necessary information simply and rapidly is vital for developing the study of implants," they wrote.