Tooth-related factors are linked to periodontal disease but systemic factors aren't, according to research presented at the recent American Association of Dental Research (AADR) meeting in Fort Lauderdale, FL. Results also indicated that older patients with mild to moderate disease are still vulnerable to bone loss, but minimally invasive treatments may reduce this risk.
Researchers analyzed patient- and tooth-related factors in periodontal maintenance patients. They found that those with progressive versus stable periodontitis had significant differences in tooth-related factors, including having open contacts between teeth, but no differences in patient-related factors such as systemic conditions, smoking, oral hygiene habits, or compliance with periodontal recalls.
"Even if you have mild disease in older patients, you need to keep watching the bone height," study author Richard Reinhardt, PhD, DDS, told DrBicuspid.com. "Some of them are still vulnerable to further breakdown. If they have open gaps between two teeth, consider restoring those."
Dr. Reinhardt is a professor of periodontology at the University of Nebraska Medical Center College of Dentistry in Omaha.
Mind the gap
Researchers from the university presented two studies at the AADR meeting based on results in the same group of periodontal maintenance patients. They started with bitewing radiographs of the patients taken before and after at least two years of periodontal maintenance.
The investigators found that while the periodontitis of these patients was generally stable, 71 of 442 patients showed at least one site with 2 mm or greater interproximal bone loss. Such patients would generally be followed in a general dental practice versus a specialty one, Dr. Reinhardt noted.
The researchers matched the 71 progressive periodontitis patients by age and gender with stable periodontitis patients (with no sites with bone loss). Patient age of these 142 matched patients was an average of 72 years and ranged from 46 to 95 years old with the bulk of patients between ages 62 and 82.
In one study, the team compared the following factors between the two groups:
- Systemic conditions from medical history: diabetes mellitus, osteoporosis, rheumatoid arthritis, and menopause
- Smoking: current smoker, former smoker, or never smoked
- Periodontal and oral disease factors: loose teeth, food or floss caught between teeth, diagnosed with gum disease, treated for gum disease, gums bleed when brush, and dry mouth
- Oral hygiene habits: brushing and flossing frequencies per week
- Compliance with periodontal recalls: number of maintenance appointments within two years and average visits per year for two years
The researchers found no significant differences at baseline between the patient groups in systemic conditions, smoking, awareness of periodontal and oral disease, oral hygiene habits, and compliance with periodontal recalls, although they found a trend toward more progressive periodontitis in patients with diabetes (p = 0.1277).
However, the investigators were somewhat surprised that 16% of the original group of 442 periodontal maintenance patients were losing significant amounts of bone, despite many of them being in their 60s and 70s.
The other study presented at AADR analyzed the following measurements in the matched progressive and stable periodontitis patients:
“Open space between the two teeth significantly increased the likelihood of progressive bone loss.”
- Cementoenamel junction to alveolar crest length
- Overhanging restorations greater than 2 mm
- Distance of restoration margin to bone crest
- Interproximal contact to alveolar crest length
- Cementoenamel junction to alveolar crest length on adjacent tooth
- Width of interproximal embrasure measured from cementoenamel junction to adjacent cementoenamel junction
- Subcontact angle (angle formed between alveolar crest to interproximal contact and adjacent tooth alveolar crest)
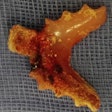
At baseline, the progressive periodontitis group had significantly smaller cementoenamel junction to bone measurement (p < 0.001) and greater interproximal width (p = 0.0016) and open contacts (p = 0.05) than the stable periodontitis group. However, the researchers found no significant differences between the groups in the other tooth-related measures.
"We had expected to find systemic risk factors, such as diabetes, and compliance with maintenance to be bigger factors, but none of them rose to the level of statistical significance," Dr. Reinhardt told DrBicuspid.com. "The anatomy around the site had a bigger impact."
The biggest issue was if the patient didn't have tooth contact, he explained.
"Open space between the two teeth significantly increased the likelihood of progressive bone loss," he said, with 42% of areas with progressive disease having open contact.
Working with this information, Dr. Reinhardt and his colleagues have established a clinic that is using minimally invasive interventions to treat progressive bone loss in periodontal maintenance patients. They are identifying patients with significant pockets that don't go away and using minimally invasive types of interventions to reduce those pockets, such as restoring gaps and performing miniflaps and papilla reflection.