Treatment with bone marrow aspirate concentrate (BMAC) may reverse the degenerative effects of osteoarthritis of the temporomandibular joint (TMJ), according to a study published in late September in the Journal of Stomatology, Oral and Maxillofacial Surgery.
Patients treated with BMAC, a procedure in which person’s own bone marrow is injected into a site of pain or injury, showed long-term joint repair after a year-plus, while those treated with hyaluronic acid relapsed, the authors wrote.
“(It) is highly suggestive that BMAC is a therapeutic modality for TMJ OA (osteoarthritis) that impedes the progression of the osteoarthritic degeneration and subsequently allowing the joint repair by providing all necessary growth factors and anti-inflammatories,” wrote the authors, led by Dina Eldahshan of Beni-Suef University in Egypt (J Stomatol Oral Maxillofac Surg, September 23, 2023).
In recent years, BMAC has been proven to be a rich source of pluripotent mesenchymal stem cells and growth factors that can significantly repair knee joints. Since BMAC can improve the joint structure, the authors wanted to assess whether it could improve the symptoms of TMJ osteoarthritis, as well as how it compared to the use of hyaluronic acid.
To explore this comparison, 24 patients who underwent joint arthrocentesis were divided into two groups. Half of the patients received intra-articular injections of BMAC, and the other half were given an injection of hyaluronic acid.
Pain levels were collected based on the visual analogue scale. Maximal mouth openings, lateral excursions, mandibular protrusion, and joint clicking were recorded preoperatively and postoperatively at one month, three months, 12 months, and 18 months.
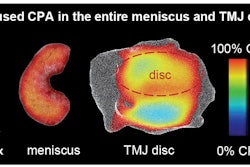
Also, patients underwent cone-beam computed tomography (CBCT) prior to injections and postoperatively at six months and 12 months. Preoperative CBCT scans for all patients showed condylar flattening, erosion, osteophytes, and narrowing of the joint space, according to the study.
Except for joint clicking, all clinical parameters showed general improvement compared to the baseline scores in those that received BMAC at 12 months and 18 months postoperatively. Initially, those who received hyaluronic acid showed improvement until six months after the procedure. These patients declined in lateral excursion and mouth opening at 12 months after the procedure. BMAC patients progressively improved throughout the study period compared to those who received hyaluronic acid, the authors wrote.
Additionally, 18 months after the procedure, CBCTs of the BMAC patients showed bony regeneration, a condylar contour that was restored to nearly normal shape, dissolution of osteophytes, and a reduction in the widening of the joint space. Except for widening of the joint space in three patients, there were nearly no changes of the osteoarthritic findings in the patients injected with hyaluronic acid, they wrote.
The results suggest that BMAC provided needed growth factors and anti-inflammatories that stopped the progression of osteoarthritic degeneration. This was contrary to the viscosupplementary action of hyaluronic acid, which resulted in patients relapsing, they wrote.
The study had limitations, including its small number of patients, the authors acknowledged. Future studies should explore the use of BMAC with a larger population and longer follow-up times, they wrote.
“Bone marrow aspirate concentrate (BMAC) is able to reverse the degenerative effects of TMJ OA,” Eldahshan and colleagues wrote.