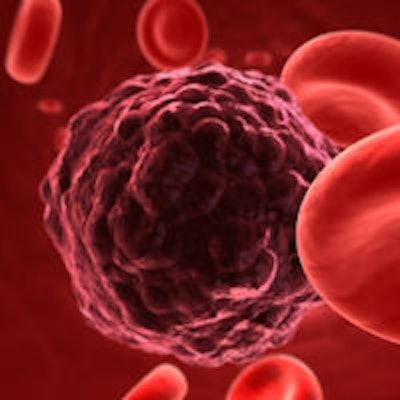
Previous research has shown that high death rates among head and neck cancer (HNC) patients usually occur only when mutations in the tumor-suppressor gene coincide with missing segments of genetic material on the cancer genome's third chromosome. Now, in a new study, researchers have found evidence suggesting that the deleterious health effects of the mutated gene may, in large part, be caused by other genetic abnormalities, at least in squamous cell head and neck cancers (Nature Genetics, August 3, 2014).
The link had not been observed before because the mutations co-occur in about 70% of head and neck tumors, and because full genetic fingerprints of large numbers of cancer tumors have only become available recently.
"These two genetic malfunctions are not two separate stab wounds to the body," stated senior co-author Trey Ideker, PhD, chief of the division of genetics at the University of California, San Diego (UCSD) School of Medicine, in a press release. "One exposes the Achilles tendon and the other is a direct blow to it."
To patients with these cancers, the study's results mean that there may be therapeutic value in testing tumors for the two genetic identifiers, known as a TP53 mutation (short for tumor protein 53) and a 3p deletion (short for deletions of genetic information on the short arm "p" of the third chromosome).
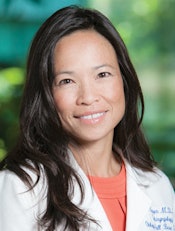 Quyen Nguyen, MD, PhD, University of California, San Diego School of Medicine. Image courtesy of UCSD.
Quyen Nguyen, MD, PhD, University of California, San Diego School of Medicine. Image courtesy of UCSD.TP53 plays a key role in regulating cell growth, detecting and fixing DNA, and directing cell apoptosis (death) if the DNA damage is irreparable. Because of this, the TP53 protein is sometimes called the "guardian of the genome."
Treatment should be intensified, the study authors suggest, if both markers are present. Treatments might be deintensified if only one mutation is present, because the TP53 mutation alone is less deadly than previously thought. Less intense treatments would likely reduce deaths from treatment complications.
"We are in the early stages of being able to personalize head and neck cancer treatments based on the tumor's actual biology, the same as what's done with breast cancers," said senior co-author Quyen Nguyen, MD, PhD, a UCSD associate professor of otolaryngology--head and neck surgery. "In the past, treatments have been based largely on the size and location of the tumor. Now, we know that some large tumors may respond to less aggressive treatment, while some small tumors may need intensified treatment. This will have a huge impact for patients."
“We are in the early stages of being able to personalize head and neck cancer treatments based on the tumor's actual biology, the same as what's done with breast cancers.”
The researchers analyzed the complete genomic signatures of 251 cases of squamous cell HNC from the Cancer Genome Atlas, a repository of sequenced cancer genomes for more than 20 different types of human cancers maintained by the National Institutes of Cancer. All the tumors were from patients younger than 85 years of age.
Of these, 179 cases had both mutations; 50 had one of the two mutations; and 22 had neither mutation. When compared with patient outcome data, independent of clinical cancer stage, half of patients with both mutations would likely die of cancer within two years, while 66% of patients with one or neither mutation would be expected to live five years or more.
Human papillomavirus (HPV) is believed to be able to co-opt the activity of TP53, affecting cells similarly to a TP53 mutation but without causing a mutation. For this reason, the researchers examined HPV-positive and HPV-negative tumors separately.
One of the study's more compelling discoveries is that among HPV-positive tumors, the most aggressive cancer cases were also highly linked to the presence of 3p deletions.
"Our findings raise fundamental questions about the role of TP53 in cancer and suggest that some of the deleterious health effects of TP53 mutations might actually be due to something else going on in the third chromosome," said lead author Andrew Gross, a graduate student in UCSD's Bioinformatics and Systems Biology Program.