Imaging aided in the diagnosis of an unusual case of aseptic necrosis of the ramus lower jaw, which developed in a man who experienced midface trauma caused by a workplace fall. The case report was published June 11 in Oral and Maxillofacial Surgery Cases.
Ultimately, the man recovered after undergoing multiple procedures that spanned more than a year. Clinicians should be aware of post-traumatic aseptic necrosis, which causes bone tissue death due to a lack of blood supply. The timing, technique employed, and strategy used can affect patient outcomes, the authors wrote.
"To the best of our knowledge, no article about traumatic necrosis of the ramus mandible is present in the literature," wrote the authors, led by Dr. Antonio Romano of Federico II University of Naples in Italy.
A 54-year-old healthy man with a jaw fracture
After an accidental fall at a workplace, a 54-year-old man lost consciousness. The man, who had no comorbidities, was admitted to a hospital and diagnosed with a left mandibular ramus fracture. He was referred to a maxillofacial surgery department.
The fall left the man with a lacerated bruised wound on his left nasal groove (which had been sutured at the hospital), swelling on the left mandibular region, as well as a lacerated bruised wound with metal clips in the lower third of his face, near the left mandible branch. Also, he had numbness in his left lower lip and chin, according to the report.
In the oral cavity, he had traumatic avulsion of the second premolar and first lower left molar, and there was mobility of some dental elements. Also, he had an open bite on the left side and a crossbite on the right side, with a maximum mouth opening limitation of 3 cm, as well as an ecchymosis in the left mucosal region, the authors wrote.
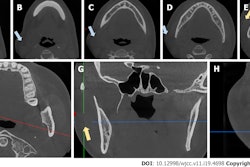
He underwent computed tomography (CT) imaging, which revealed a continuous solution of the left submandibular region of the cutaneous and subcutaneous layers extending from the condylar to his cheek area. Abundant air detached the perivascular and parapharyngeal adipose layers, and the subcutaneous emphysema extended homolaterally to the laterocervical region. Also, clinicians reported a displaced fracture, with diastasis of the fragments with a branch of the left mandible, according to the report.
 A CT scan revealed axial (a) and coronal (b) sections showing aseptic necrosis of the ramus mandible. Images courtesy of Romano et al. Licensed by CC BY 4.0.
A CT scan revealed axial (a) and coronal (b) sections showing aseptic necrosis of the ramus mandible. Images courtesy of Romano et al. Licensed by CC BY 4.0.The patient underwent an open reduction and internal fixation. Within the oral cavity, a wound with an exposure of the left mandibular branch was found, as well as a large amount of necrotic muscle tissue. The necrotic tissue was found externally at the lower head of the internal pterygoid muscle and internally at the upper head, they wrote.
 A 3D image shows the left mandibular ramus fracture.
A 3D image shows the left mandibular ramus fracture.Surgeons used the original wound to expose the ramus fracture. Rigid fixation was achieved by means of a six-hole 2-mm and a six-hole 2.4-mm locking titanium plate after an intermaxillary block. Drainage was placed in the left hemimandibular region due to the necrosis.
After the procedure, CT scans showed a correct reduction of the patient's fracture. Also, the man was given antibiotics for seven days.
 A 3D image shows a correct reduction of the left mandibular ramus fracture after surgery.
A 3D image shows a correct reduction of the left mandibular ramus fracture after surgery.During outpatient follow-up one month later, the man had swelling in the hemimandibular region. Therefore, he was hospitalized and underwent a CT scan, which showed swelling and thickening of the soft tissues of the left cheek and submandibular region, as well as evidence of fluid collection in the homolateral masseter muscle and analogous fluid collection on the mesial side of the mandibular angle, the authors wrote.
After infectious disease counseling, the man underwent treatment antibiotics and a beta-lactamase inhibitor. Unfortunately, it was necessary to perform surgery to remove the internal fixation system. During this procedure, purulent matter was found, a fistulectomy was performed, and a sample was sent for lab testing, they wrote.
A month later, surgical debridement was completed. Curettage of the bone cortex was performed by means of rotating and removing the condylar bone fragments.
About one year and six months after the first surgery was performed, swelling was found in the man's left mandibular corner. A CT scan revealed a morphostructural alteration of the patient's upper two-thirds of the vertical branch of the neck, of the coronoid process and of the mandibular condyle, the authors wrote.
In addition, skin discontinuity with partial bone exposure and an uneven appearance of the subcutaneous plane were observed at the level of the ipsilateral mandibular angle. Therefore, surgeons performed an osteotomy on the healthy bone segment and removed the necrotic mandibular angle.
Approximately six months after the last surgery, clinicians observed the man's optimal locoregional conditions of the surgical wound, and he had a mouth opening of more than 3 cm, they wrote.
Why this case matters
Also known as osteonecrosis and avascular necrosis, aseptic necrosis occurs when vascularity is severely affected. Though this condition can involve any bone, more often, it develops in the jaw. If left untreated, it can be life-threatening.
In the literature, most cases of aseptic necrosis are linked to bisphosphonates, a class of drugs used to prevent or curb bone loss, and the condition is described as an emerging oral complication in oncology patients, according to the report.
In addition to not finding cases of post-traumatic aseptic necrosis in the literature, the authors wrote that there have been only four reported cases of traumatic maxillary necrosis.
There are several physiological variations within the maxillary artery and its course, including whether it travels lateral or medial to the lateral pterygoid muscle. Studies have shown that there is a 66% chance that the artery travels laterally and a 33% chance that it travels medially, they wrote.
Surgeons should consider these variations when performing bilateral operations, such as a bilateral condylectomy, gap arthroplasty, or internal fixation of a bilateral subcondylar fracture. For treatment planning purposes, clinicians should be aware that artery tears can occur due to their close relationship between the maxillary artery and the mandible, Romano and colleagues wrote.
"Although the artery may not have been damaged during the initial trauma, its proximity to the edges of the fracture puts it in constant danger of being torn by subsequent movement of the fractured bone ends," the authors wrote.