Oral surgeons should be aware of a rare, serious oral fungal infection that may occur after COVID-19 treatment, according to a case report from Tennessee published on September 19 in the Journal of Oral and Maxillofacial Surgery.
The 75-year-old man described in the report underwent several procedures, including the extraction of multiple teeth, removal of zygomatic and maxillary bone, and exenteration of his eye, to treat his rhinocerebral mucormycosis, also known as black fungus.
"Oral-maxillofacial surgeons (OMSs) should be aware of this rare disease, especially as COVID-19 patients are becoming more likely to survive their initial illness and develop sequelae of this disease and its treatment," wrote the authors, led by Dr. Andrew Deek, a resident physician in the oral and maxillofacial surgery department at the University of Tennessee Medical Center in Knoxville.
Unusual but serious
Native to the Middle East and India, Mucor is a type of fungus commonly found in fruit and soil. Its spores can be inhaled into the body, leading to mucormycosis. Most encounters do not lead to infection, but immunocompromised patients, such as those with uncontrolled diabetes, are at greater risk.
Since the spring of 2021, India has reported a marked increase in mucormycosis of the head and neck. Patients with uncontrolled diabetes who were treated recently for COVID-19 often become infected.
Dexamethasone is commonly used to treat COVD-19, but it also makes patients more susceptible to secondary infections. As the novel coronavirus continues to infect people across the U.S., oral and maxillofacial surgeons should be aware of mucormycosis so that treatment is not delayed, according to the authors.
A patient with multiple underlying conditions
In January 2021, a 75-year-old man with a past medical history of poorly controlled type 2 diabetes, coronary artery disease with remote history of myocardial infarction, and atrial fibrillation presented to a hospital in east Tennessee with altered mental status. When he arrived, he was found to be in atrial fibrillation with rapid ventricular response and diabetic ketoacidosis, the authors wrote.
He was transferred to another hospital for admission to the intensive care unit. He was in mild distress and had left eye conjunctivitis. Initially, a rapid COVID-19 polymerase chain reaction (PCR) test came back negative, but a chest x-ray showed bilateral pneumonia.
He was admitted to the hospital and underwent an oropharyngeal COVID-19 test, which came back positive. The patient began receiving dexamethasone and was given one unit of convalescent plasma. After six days of treatment, he was discharged because he no longer had respiratory symptoms or oxygen requirements, and his white blood cell count was no longer elevated, they wrote.
Five days later, the man returned to the hospital with worsening facial swelling, subjective fever, and decreased visual acuity in his left eye, and his conjunctivitis had worsened, the authors noted.
Due to concerns that he had a left facial abscess, he was transferred to the department of oral and maxillofacial surgery. The man underwent a maxillofacial computed tomography (CT) scan that showed severe soft-tissue emphysema that extended throughout his left cheek from the inferior aspect of his left maxilla superiorly to the level of his left orbit, anteriorly to the base of his nose, and posteriorly to his left masseter muscle.
Also, his left eye was bulging, which appeared to be linked to preseptal cellulitis, fluid, or conjunctivitis causing external compression on the left orbit, as well as left maxillary osteomyelitis, they wrote.
Lab results showed that he had high red and white blood cell counts, and a physical exam showed that the pupil in his left eye was nonreactive, along with left facial cellulitis with crepitus. The patient was sent to the operating room for incision and drainage, debridement of the left side of the face, and extraction of three teeth.
During the procedure, clinicians discovered that his maxillary and zygomatic bone appeared necrotic. These areas were debrided and sent for lab analysis, and the patient was started on ceftriaxone, vancomycin, and metronidazole.
After the procedure, he was sent to another department for medical management and was scheduled for infectious disease and ophthalmology consultations. Additionally, the results from the samples taken during the procedure were positive for Enterococcus faecalis, multiple-drug-resistant Escherichia coli, and Prevotella, and the patient was prescribed antibiotics.
Two days later, oral and maxillofacial surgeons took him back to the operating room to further debride necrotic tissue and drain new abscesses in his left anterior temporal space and masseteric space. During this procedure, they discovered significant soft-tissue necrosis of the masseter and buccinator.
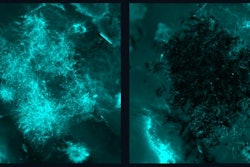
Bone pathology revealed that the patient had extensive necrosis of his left maxilla and zygoma caused by fungi and bacteria, suspected to involve Mucor. He was treated with amphotericin B, which is reserved for life-threatening fungal infections, the authors wrote.
At this point, his white blood cell count was no longer elevated, and CT confirmed that pre- and postseptal cellulitis had resolved. Fungal cultures eventually revealed the presence of Mucor.
The next week, the man underwent multiple washout and debridement procedures. Evolving necrosis was found from his lateral orbital wall through the zygoma, maxilla, and hard palate and involved soft tissue, including buccinator, masseter, and buccal mucosa. Later, clinicians found that the fungus had invaded the man's ethmoid and sphenoid sinuses, and he was prescribed isavuconazonium along with liposomal amphotericin B.
Due to the extent of the necrosis, otolaryngology was consulted. Clinicians performed an exenteration of his left eye and debridement of his midface and anterior skull base, the authors wrote.
A long road to recovery
Because the wound and involvement of his frontal, maxillary, and sphenoid sinuses were extensive, a segment of his thigh was used for reconstruction. Tissue flaps from his thigh were also used to cover the eye area. The patient continued antifungal treatment for several months, the authors wrote.
After spending 109 days at the University of Tennessee Medical Center, the man was transferred to a skilled nursing facility. Two months later, he had fully recovered and had no postoperative complications, the authors wrote.
Mucormycosis may increase as the COVID-19 pandemic continues; therefore, specialists who treat head and neck infections, including oral and maxillofacial surgeons, must be aware of the disease.
"There will be a role for the dental community, especially OMSs, to identify these cases before significant morbidity or mortality occurs," Deek and colleagues wrote.