A record number of eligible children are participating in Medicaid or the Children's Health Insurance Program (CHIP), according to new data from Health Affairs. As of 2016, nearly 94% of eligible children were enrolled in the programs.
Since the passage of the Patient Protection and Affordable Care Act (ACA) in 2010, Medicaid/CHIP enrollment has been steadily increasing for eligible children. The researchers attributed the growth of children's participation to insurance expansion and also outreach, enrollment, and renewal efforts.
"Uninsurance rates among U.S. children fell by more than 60% over the past two decades, following expansions of public health insurance under Medicaid, the Children's Health Insurance Program, and the Affordable Care Act, and accompanying investments in outreach, enrollment, and renewal processes," wrote the researchers, led by Jennifer Haley, a research associate in the Urban Institute's Health Policy Center in Washington, DC (Health Affairs, August 6, 2018). "Uninsurance rates for adults also fell following implementation of the ACA's coverage provisions but remained higher than the rates for children."
Coverage reaches record high for kids
Medicaid and CHIP provide insurance coverage, including dental insurance coverage, for almost 40% of U.S. children, according to data from Families USA, a nonprofit healthcare advocacy organization. Furthermore, since the ACA passed, more children without other insurance options are enrolling in Medicaid or CHIP, and the number of uninsured children has continued to decrease.
The new research shows 2016 was no exception to these trends. Using data from the American Community Survey (ACS), an annual survey from the U.S. Census Bureau, Haley and colleagues found that 93.7% of eligible children without other insurance options were enrolled in Medicaid or CHIP in 2016. This was the highest level of Medicaid/CHIP participation since the researchers began tracking the data in 2008, and it is 5% than higher than the coverage rate for children in 2013.
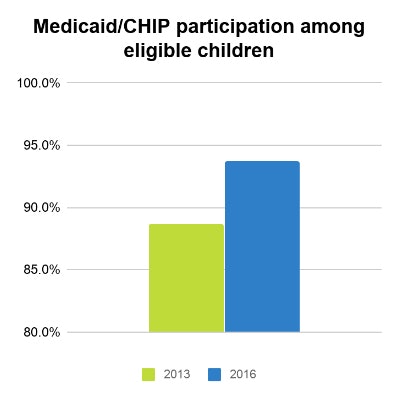
"Children's participation in Medicaid/CHIP rose between 2013 and 2016, which suggests that continued policy efforts to improve outreach, enrollment, and retention and the implementation of the ACA's coverage provisions succeeded in reducing the number of eligible but uninsured children," the researchers wrote.
While more eligible children are participating in Medicaid/CHIP than ever before, Medicaid participation is growing at a slower rate for parents and childless adults, and adult participation varies greatly by state. For instance, fewer than 60% of eligible parents in Alaska, Georgia, Nebraska, Oklahoma, and Texas participated in Medicaid, while more than 94% of eligible parents in Massachusetts and Vermont participated.
"Participation among parents and childless adults remained lower than among children, and eligible uninsured adults outnumbered eligible uninsured children," the researchers wrote. "This points to the key role that enrollment increases among Medicaid-eligible adults could play in achieving additional coverage gains across the country."
Unclear if growth will continue
The Health Affairs analysis had a number of shortcomings, notably that survey participants self-reported their coverage status, and, therefore, the data are subject to measurement error, the researchers noted. In addition, data limitations made it difficult to estimate Medicaid eligibility for adults, and the researchers could not provide participation estimates for childless adults in states that did not expand Medicaid due to varying coverage requirements.
Furthermore, while the number of children accessing insurance has continued to hit record highs, that may change in the future. Current trends, such as the slowing of Medicaid enrollment growth, changes to eligibility rules and requirements, and new states expanding the program, may all factor into future participation numbers, the researchers noted..
"Reduced funding for general ACA outreach and enrollment efforts and new restrictions in state Medicaid eligibility and enrollment rules may create uncertainty about coverage options and other barriers, which, in turn, could hamper enrollment," they wrote. "Finally, while the elimination of federal individual mandate penalties is predicted to reduce Medicaid/CHIP coverage in 2019. Medicaid expansion under the ACA, which is being considered in additional states, could increase enrollment among childless adults, parents, and children in those states."