
Dental therapists increased profits, patient visits, and the number of new patients at two practices, one in the U.S. and one in Canada, according to a new Pew Charitable Trusts report that analyzed their impact on the practices' bottom lines and productivity.
The dentists who hired the midlevel providers (MLPs) also praised their abilities in the report, noting that having MLPs perform routine procedures gave the dentists more time for complex treatments.
"Expanding the Dental Team" examines two private dental practices that employ dental therapists (DTs) to increase access to dental care for underserved populations. One of the practices is in rural Minnesota and was the first private practice in the U.S. to hire a DT. The other practice is in the Canadian province of Saskatchewan, where the dentist hired a DT more than 30 years ago.
Difficulties in accessing dental care, especially for low-income people, have been well-documented. For instance, in 2009, more than 830,000 dental-related visits to U.S. emergency rooms could have been avoided with earlier care, the report states. In 2011, more than half of all children on Medicaid did not see a dentist.
More than 50 countries have improved access to dental care by allowing providers other than dentists to offer routine preventive and restorative care, according to the report. When compared with dentists, these midlevel providers -- DTs and hygienists with extra training in restorative care -- require less education, perform fewer procedures, and receive lower salaries.
Research has confirmed that they provide high-quality, cost-effective routine care and improve access to treatment in parts of the country where dentists are scarce, the authors wrote. In the U.S., MLPs are now working in Alaska and Minnesota, and 15 states are considering licensing them to do similar procedures.
The report included Canada because its dental care delivery system is similar to that of the U.S., with residents obtaining private dental insurance or paying out of pocket for care. Also, the Canadian office illustrated a mature practice model.
Findings
Pew's analysis of the two practices determined the following:
Significant numbers of underserved patients were able to get care, and the practices continued generating profits. Profit levels were influenced by factors such as the size of the patient population receiving government subsidies for care and the amount of the subsidies.
Dentists were able to focus on more-complex procedures that generate higher revenue. Using DTs to perform routine restorative care allowed the dentists to concentrate on advanced procedures such as crowns and bridges.
The U.S. practice analyzed was Main Street Dental Care, a solo practice in Montevideo, MN, (a town of about 5,300 people) operated since 2000 by John Powers, DDS. Dr. Powers also teaches at the Rice Regional Dental Clinic, a training site for the University of Minnesota's dentistry, dental hygiene, and DT students, the report noted.
Minnesota began allowing DTs and advanced DTs to practice in 2009. Currently, there are 25 such providers practicing in the state. In February 2012, Dr. Powers hired a dental therapist to work in his practice three days per week.
An analysis of Dr. Powers' records showed that revenue and the number of visits, new patients, and surgical procedures performed by him have increased since adding a DT, while the number of nonsurgical services he performed decreased.
In the year following the dental therapist's arrival:
- Patient visits increased by 27%; new patients increased by 38%.
- The number of Medicaid patients increased from 26% in 2011 to 39% in 2012.
- Patient billing increased by 33%.
- After accounting for the cost of employing the DT, profits increased by $23,831.
Dr. Powers hired dental therapist Brandi Tweeter who had worked as a dental assistant in his practice for more than a decade. When she expressed an interest in furthering her dental education, Dr. Powers said he would take her into his practice after she completed her studies. That year, Tweeter entered the 28-month dental therapy program at the University of Minnesota, graduating in 2011. Before entering the program, she had a bachelor's degree in biology.
Some patients were skeptical of a DT doing restorations, but their concerns soon faded, Dr. Powers said.
Because Minnesota law requires that at least half of a DT's patients be underserved, the practice started accepting more Medicaid patients in preparation for Tweeter's arrival. By the end of 2012, 62% of Tweeter's patients and 39% of overall practice patients were on Medicaid.
"I have people coming to me from as far as two and a half to three hours away," Tweeter said in the report.
Dr. Powers does initial patient exams to determine necessary treatment. Tweeter sees five to 10 patients daily, mostly for composite restorations and primary tooth extractions. All children's restorative care is scheduled with Tweeter, according to the report.
The number of procedures performed at the office increased by 27% (2,062) between 2011 and 2012; Tweeter was responsible for nearly half (972).
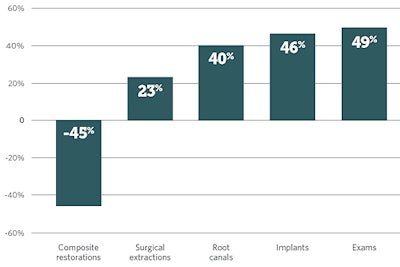 Change in common procedures performed by Dr. Powers, 2011-2012. Data from Main Street Dental Care, December 2, 2013. All images courtesy of Pew Charitable Trusts.
Change in common procedures performed by Dr. Powers, 2011-2012. Data from Main Street Dental Care, December 2, 2013. All images courtesy of Pew Charitable Trusts.Medicaid reimbursements increased from 41% of Dr. Powers' usual charges to about 55% after the practice qualified as a "critical access dental provider" in 2013. The qualification includes providers in dental shortage areas who serve substantial numbers of Medicaid patients.
In 2012, Tweeter worked 25 hours per week at $45 per hour, practicing when Dr. Powers was onsite. The practice's employment cost for Tweeter for her first 11 months -- including salary, benefits, taxes, overhead, and the partial time of a dental assistant -- totaled $90,671. During that time, she billed $156,078 in patient care.
 Dental therapist's fiscal impact, 2012. Data are from Main Street Dental Care and are for 11 months, from February through December 2012. **Tweeter’s procedure volume in her first few months of employment was significantly lower than in subsequent months.
Dental therapist's fiscal impact, 2012. Data are from Main Street Dental Care and are for 11 months, from February through December 2012. **Tweeter’s procedure volume in her first few months of employment was significantly lower than in subsequent months.After accounting for the cost of employing Tweeter, practice profits increased by $23,831.
"Tweeter increased procedure volume and provided care at a lower cost than if Dr. Powers had performed the same procedures," the authors of the report concluded.
A longer DT history
The second practice the report reviewed was Battlefords Dental Group, a private practice founded by Lornce Harder, DDS, in 1965. Two DTs work there; one was hired in 1980 and the other in 2009. The practice is located in North Battleford, a rural town of about 14,000 people in west-central Saskatchewan. About 20% of the area's population is from indigenous communities, according to the report.
Dental therapists have been practicing in Saskatchewan since 1974. Originally, they worked in schools or served indigenous people in rural northern areas of the province. As of 2013, more than half (144) of the province's 235 dental therapists worked in private practice. The others were employed by health departments and agencies that serve indigenous populations.
In the report, Dr. Harder said that DTs have freed him to focus on crowns, bridges, surgeries, and other advanced procedures by handling the practice's routine restorative care. Practice records showed that DTs generated combined profits of $197,329, after accounting for commissions and other overhead expenses.
“Darcy has become so specialized that I wouldn't want to pretend that I could touch the work that she does in fillings because I haven't done it for a long time.”
About 85% of Dr. Harder's collections come from private insurance or self-pay, 10% come from government payments for indigenous patients, and 5% come from government payments for welfare recipients. The federal government's Indian Health Service reimbursement rate is 85% of the Saskatchewan Dental Association's fee schedule -- approximately 12% of the practice's patient base is indigenous -- and the provincial government reimburses for patients on welfare at 70% of provincial dental retail fees.
Dr. Harder hired Darcy Tkatchuk as a dental therapist in 1980. She is licensed as both a DT and a hygienist, having completed a two-year training program for dental therapy and a 10-month program for dental hygiene. In 2009, Dr. Harder hired Siri Bounlom as the practice's second dental therapist.
The DTs split their time between providing dental therapy services and preventive services, the report noted.
Dr. Harder had supervised a DT training program and was impressed with the education the students received and their overall competence, according to the report. One of the reasons he hired Tkatchuk was that he wanted to hand over care of many of the children in his practice and knew her experience working in a school-based program would be advantageous.
Like Dr. Powers, Dr. Harder sees all patients for initial exams. Most of Tkatchuk's work involves restorations, but she also performs procedures such as sizing night guards, prepping for orthodontics, and extracting primary teeth.
Dr. Harder and Tkatchuk work four days a week. She works about 30 hours a week and sees eight to 14 patients a day, including children and adults.
"Sometimes when I am away and I want patients to be looked after, I will let [Tkatchuk] do the checkup. She can discern cavities just as well as I can," Dr. Harder said in the report. "Darcy has become so specialized that I wouldn't want to pretend that I could touch the work that she does in fillings because I haven't done it for a long time."
Tkatchuk and Bounlom have different salaries when they work as hygienists -- primarily handling prophys, scaling, polishing, and fluoride application -- than they do for procedures as therapists. They are paid exclusively on commission, receiving 40% on all billings for hygiene services and 35% (for Tkatchuk) or 30% (for Bounlom) for DT services. Dr. Harder gets a 10% commission on all services provided by the therapists. DT services are billed at rates that are two to four times higher than hygiene services.
In 2012, combined collections from the two DTs totaled $481,107, about half from hygiene services. After subtracting their commission, $174,635, the DTs brought in $306,472. The practice did not incur additional employment costs for the DTs, the report noted. The combined services provided by the DTs equaled 54% of total practice collections in 2011 and 2012.
After overhead costs, they contributed an estimated $197,329 to practice profits. The practice was able to generate this profit even though a substantial portion of billings -- about 15% percent of revenue -- was paid at discounted government rates.
"What I value the most is to see work that lasts sometimes for more than 10 years," Tkatchuk said in the report.
Conclusion
"Findings from two practices cannot be conclusive about the potential financial benefit for dental practices of employing dental therapists or how they can employ midlevel providers to increase access to care in the communities in which they work," the report authors acknowledged.
"These case studies demonstrate, however, that for private dental practices, using midlevel providers can be a good business decision that addresses the access gap for low-income individuals and can enable dentists to focus on the complex procedures that only they have the skills to perform," they concluded.



















