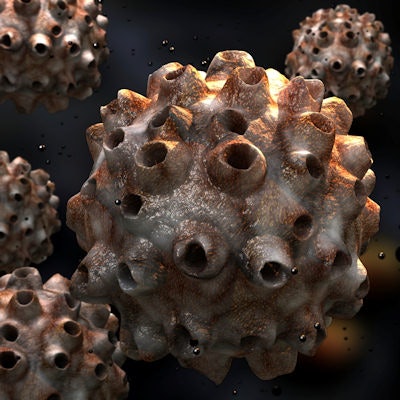
Human papillomavirus (HPV) vaccination programs have a substantial impact on the number of infections in girls and women, according to a study published on June 26 in Lancet.
Researchers updated a systematic review and meta-analysis to include data from 60 million individuals and up to eight years of follow-up. They reported that the prevalence of HPV strains 16 and 18, which cause 70% of cervical cancers, decreased by 83% among girls ages 13 to 19 and decreased by 66% among women ages 20 to 24 five to eight years after vaccination.
"Our results provide strong evidence that HPV vaccination works to prevent cervical cancer in real-world settings as both HPV infections that cause most cervical cancers and precancerous cervical lesions are decreasing," stated lead author Mélanie Drolet, PhD, an epidemiologist and senior research associate at Laval University in Quebec City, in a Lancet press release.
The researchers conducted a systematic review and meta-analysis of the population-level effect of vaccinating girls and women against human papillomavirus on HPV infections, a diagnosis of anogenital warts, and cervical intraepithelial neoplasia grade 2+ (CIN2+) in high-income countries. They included 65 articles in their analysis.
The prevalence of five strains of HPV dropped during the follow-up period (see table below).
| Percentage decrease of HPV, anogenital warts, and CIN2+ on follow-up | |||
| Condition or diagnosis | Ages 13 to 19 | Ages 20 to 24 | Ages 25 to 29 |
| HPV strains 16, 18 | 83% decrease | 66% decrease | |
| HPV strains 31, 33, 45 | 54% decrease | ||
| Anogenital wart diagnosis | 67% decrease (ages 15 to 19) |
54% decrease | 31% decrease |
| CIN2+ | 51% decrease (ages 15 to 19) |
31% decrease | |
The authors noted some study limitations, including that causality between the vaccination and the observed changes could not be concluded definitively because the analysis is based on ecological studies. They were also unable to define the impact of specific program characteristics, such as what vaccine was used, number of age cohort population vaccinated, and more.
However, they concluded that the results provide strong evidence of HPV vaccination working to prevent cervical cancer in real-world settings, as both the cause (high-risk HPV infection) and proximal disease endpoint (CIN2+) are significantly declining.


















